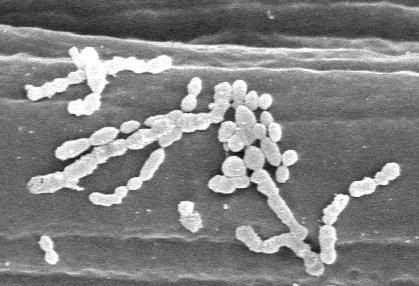
 Speaking of chronic diseases caused by microbial agents, one of the earliest characterized of these is the group A streptococcus (Streptococcus pyogenes). In addition to causing acute diseases such as strep throat and scarlet fever, a wide range of post-infectious sequelae (complications that appear following resolution of infection) have been attributed to S. pyogenes. It can cause glomerulonephritis, a kidney disease. It's long been known infection with the organism can lead to a condition called Sydenham's chorea, a neurologic disease characterized by jerky movements. Infection with S. pyogenes has also been linked to a number of related syndromes, including Tourette's syndrome and tic disorders. Most notably, S. pyogenes causes rheumatic fever, a disease that affects multiple organ systems. Rheumatic fever can lead to damage of the heart valves, resulting in a condition known as rheumatic heart disease. It is thought that this is due to cross-reaction of antibodies against the bacteria: they also react with heart tissue. The recognition that the bacteria causes these diseases is a reason it is recommended that streptococcal infections be rapidly treated with antibiotics, as this significantly decreases the incidence of RF.
Speaking of chronic diseases caused by microbial agents, one of the earliest characterized of these is the group A streptococcus (Streptococcus pyogenes). In addition to causing acute diseases such as strep throat and scarlet fever, a wide range of post-infectious sequelae (complications that appear following resolution of infection) have been attributed to S. pyogenes. It can cause glomerulonephritis, a kidney disease. It's long been known infection with the organism can lead to a condition called Sydenham's chorea, a neurologic disease characterized by jerky movements. Infection with S. pyogenes has also been linked to a number of related syndromes, including Tourette's syndrome and tic disorders. Most notably, S. pyogenes causes rheumatic fever, a disease that affects multiple organ systems. Rheumatic fever can lead to damage of the heart valves, resulting in a condition known as rheumatic heart disease. It is thought that this is due to cross-reaction of antibodies against the bacteria: they also react with heart tissue. The recognition that the bacteria causes these diseases is a reason it is recommended that streptococcal infections be rapidly treated with antibiotics, as this significantly decreases the incidence of RF.
The epidemiology of S. pyogenes infections in the 20th century has been interesting. At the beginning of the 20th century, scarlet fever was still a scourge, with mortality rates as high as 30% in some outbreaks. This started to decline in the early quarter of the century, and is currently considered a mild consequence of S. pyogenes infection. Rheumatic fever also caused significant morbidity and mortality until the 1950s, when it began to decrease (largely due to an increased use of antibiotics to treat strep throat infections). In the 1970s, the incidence of rheumatic fever in the United States further declined, followed by a resurgence in some areas during the 1980s. At the same time, the incidence of severe invasive disease due to S. pyogenes (including streptococcal toxic shock-like syndrome [STSS] and necrotizing fasciitis, the "flesh-eating disease") also increased. How much of this was due to changes in the pathogen, versus changes in the environment or the host, has been the subject of much study.
Strains of S. pyogenes appear to have different disease potential, which in turn relate to their genetic make-up. This also seems to correlate with their tissue preference. While strep throat is the most common disease manifestation in the United States, it is also a common cause of a skin disease called impetigo. This disease is more common in troical climates. Bessen et al. have shown that this tissue preference appears to have a basis in differences in the emm gene, which encodes the M protein--a key virulence factor, and the determinant of serotype. Additionally, isolates that cause skin infections are infrequently associated with subsequent development of rheumatic fever, but are more commonly a cause of glomerulonephritis. Instead, RF is generally associated with prior infection in the throat. However, not all throat isolates cause RF; only a subset of them typically do. (Are you seeing why studying the epidemiology of these organisms is exhausting?) Those that cause RF typically lack a gene called sof, encoding a protein called the serum opacity factor. RF-causing isolates also typically produce large amounts of capsule, a sticky extracellular polysaccharide.
I've noted before that the development of disease due to an infectious agent results from a complex interaction of host genetics, microbial genetics, and environmental factors (which can include host nutrition and immune status, among other things). In the case of rheumatic fever, only a subset of types of S. pyogenes bacteria generally cause rheumatic fever. As I mentioned above, the incidence of RF has changed over the years. The initial decrease could be attributed to antibiotics, but what about the decrease seen the in 1970s? Or the increase in some areas in the 1980s? A new study examined their changing epidemiology.
In the US, the incidence of rheumatic fever has dropped dramatically over the past 4 decades (see figure).  Was this due to a change in the population structure of S. pyogenes? Previous studies had suggested it was. To test this, Shulman et al. examined the M type of bacteria collected between 1961-8 in Chicago, and from Chicago and a number of other sites across the country between 2000-4. 2 types that are known to cause rheumatic fever (serotypes 1 and 12) had essentially identical percentages over the years and in various geographic regions. However, other rheumatogenic seroypes--3, 6, 5, and 14--were significantly decreased in the recent sampling compared to those found in the 1960s. Other nonrheumatogenic types, conversely, increased, including serotypes 2, 4, 22, and 28.
Was this due to a change in the population structure of S. pyogenes? Previous studies had suggested it was. To test this, Shulman et al. examined the M type of bacteria collected between 1961-8 in Chicago, and from Chicago and a number of other sites across the country between 2000-4. 2 types that are known to cause rheumatic fever (serotypes 1 and 12) had essentially identical percentages over the years and in various geographic regions. However, other rheumatogenic seroypes--3, 6, 5, and 14--were significantly decreased in the recent sampling compared to those found in the 1960s. Other nonrheumatogenic types, conversely, increased, including serotypes 2, 4, 22, and 28.
So, this suggests that a decrease in rheumatogenic serotypes of S. pyogenes has played a role in the decreasing incidence of rheumatic fever in the United States over the past 40 years. However, rheumatogenic M types have decreased only approximately 2-5 fold, while RF has decreased approximately 20-fold--so we're still not seeing the whole picture. These missing pieces become critical because a vaccine for S. pyogenes based on the M protein is in the works. Though this is a main antigen, it's been tough to design a vaccine against it due to the fact that antibodies to the protein cross-react with heart tissue--an autoimmune reaction that results in the development of RHD. Though this disease is now rare in the US and other developed countries, it is still a scourge worldwide. Chronic RHD is estimated to exist in 5-30 million children and young adults; 90,000 patients die from this disease each year.
This study also highlights the value of surveillance. Especially when designing a vaccine, we need to know what's out there, how the population has changed, and ideally, what's caused that change. Then when the vaccine is implemented, we need additional surveillance to look for emergent strains that may replace those contained in the vaccine. For example, following the introduction of the vaccine against Haemophilus influenzae type B, rates of meningitis caused by this bacterium have decreased dramatically. However, we're now seeing more non-type B isolates of Haemophilus--so a vaccine for a particular pathogen doesn't always represent the end of the story.
One final thought: though it appears that a change in circulating serotypes of S. pyogenes has played a role in the decline of rheumatic fever in the United States, we don't know what factors caused some of these serotypes to become more dominant, and others to become increasingly rare. That's a very difficult task to figure out. It could be that the strains that took over simply out-competed the strains that are now unusual; it could be due to other bacterial agents that share the same niche; it could be due to man-made agents (perhaps some are more resistant to antibiotics, or antimicrobial chemicals, even soaps, etc.), or it could be due to a number of other things. This is one of the things that makes studying this area so difficult. Imagine the challenge "regular" ecologists have when they look at changes in the ecology of an area. Now imagine that everything they're studying is invisible to the naked eye, and some can be investigated only by DNA-based methods. It's a challenging, but fascinating, area.
Article: Shulman ST et al. 2006. Temporal Changes in Streptococcal M Protein Types and the Near-Disappearance of Acute Rheumatic Fever in the United States. CID. 42:441-447.
Picture from here.
- Log in to post comments

Nice article (you knew I'd have to say something). The necrotizing fasciitis case just recently got more interesting with the recent description of cases from community acquired MRSA. It would be very interesting to know why TSS and NF occur. By that I mean, why does production of SpeA cause STSS sometimes, and NF other times. Now that the same thing is starting to occur w/ staph, it seems unlikely that it is something special about that toxin. It seems more likely that there is some additional factor at work. You may know more about that than I, since I was focused on toxins themselves.
The genetics is really neat too. I recall Musser did a lot of work on comparative genomics of streps. I don't recall what the big picture story was.
The big picture is still somewhat of a mess. I just attended a talk by Victor Nizet (in whose lab the work described in this post was carried out), and he said that Musser has a paper coming out that tries to synthesize things a bit more.
Actually, I think it was this paper he mentioned, which is just out today.
Ask and you shall receive, or something like that. Nice paper, that. Everytime I see something like that I get more and more depressed about how slow my own stuff seems to go...
As one of the 150 or so people who got rheumatic fever in 1971, I'd be thrilled to know that my chances of a recurrence are going down as time goes by. Here's one endangered species (sic) that I'd be happy to see gone today!
My 11 year old son for RF this last spring. It started with a fever that lasted 3-4 weeks, coming and going rash, really really really bad arthritis, swollen digit and a few other symptoms. I had to take him out of school for 2 1/2 months and it was a very trying time for us all especially him.
He's taking 2 penicillian pills a day till he's 21 now.
I've taken a quick look at your postings, which are very interesting. Lots of material and ideas! Congrats on being so focused!
The advice given in your blog is fantastic and very complimentary to my site, check it outBest kept secrets
Great collection of posts and thanks for recognizing the ethics issue. We are starting the discussion on what, if any, standards should be developed. Please weigh in.
I look forward to your future work.
This is a great article. I am new to your blog and i like what I see. I look forward to your future work.